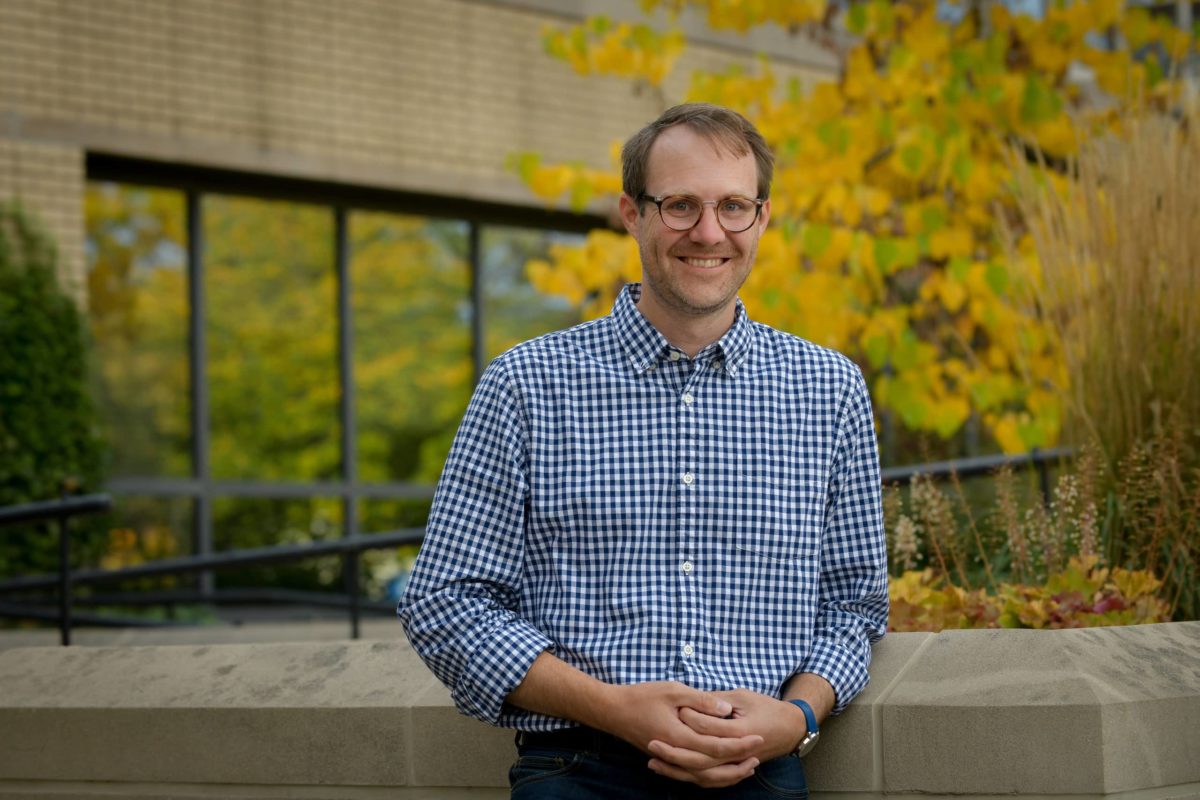
Medical Role Models Matter
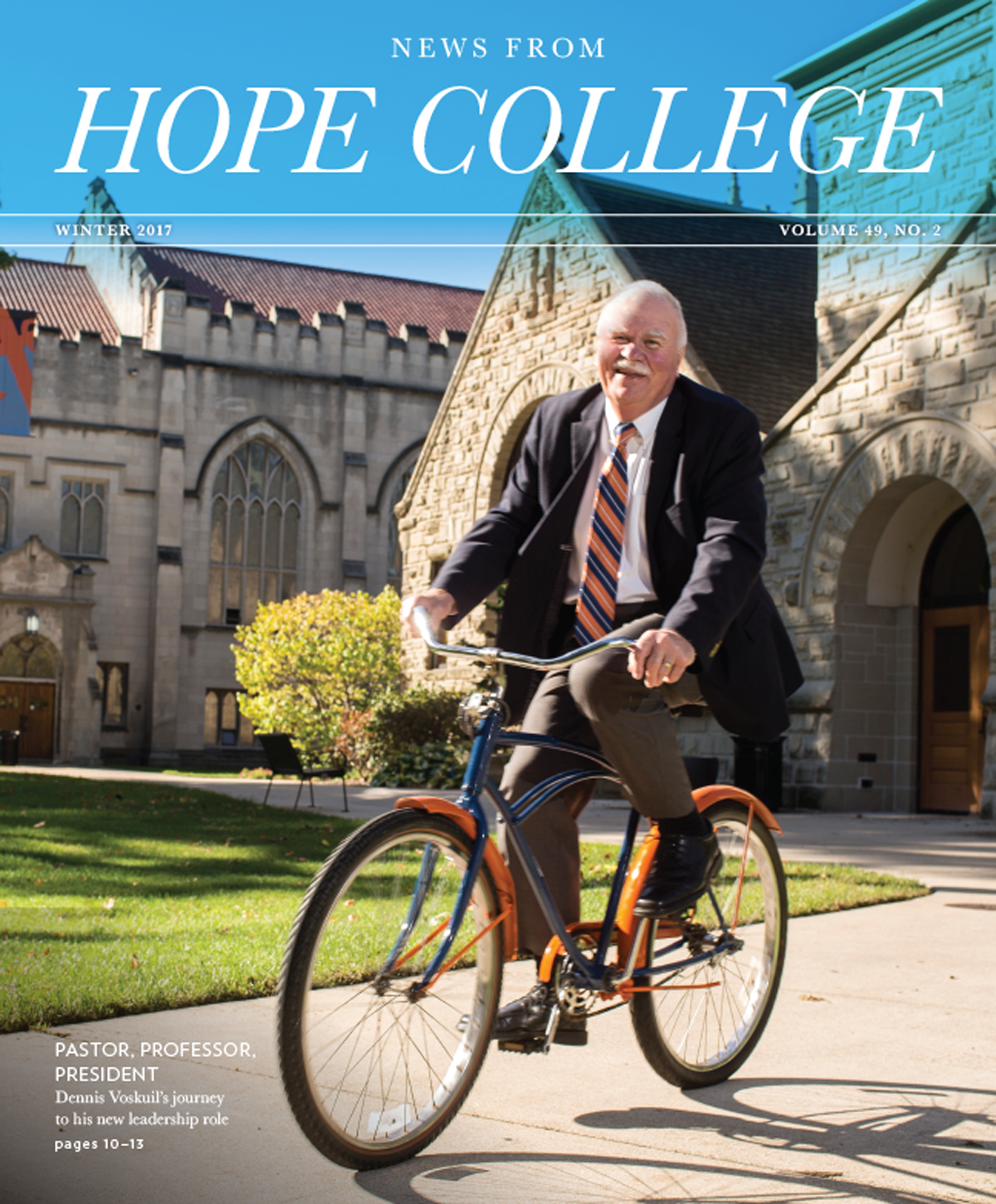
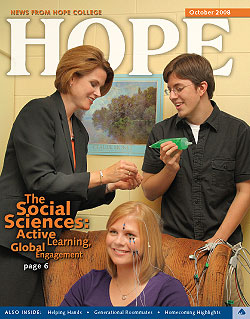
Aaron Franzen, Ph.D. | Associate Professor of Sociology
Dr. Aaron Franzen has been curious for years about the “hidden curriculum” of medical schools — the undercurrent of norms and expectations for behavior that medical students learn outside their official curriculum. “It’s the social water in which all of them swim, so it matters — whether they recognize it or not,” he says.
Until now, most research on medical socialization has focused on negative consequences of exposure to such norms and values, he reports. In a study, Franzen investigated the flip side in hopes that documenting what has a positive impact will motivate medical educators to do more of it.
He found that simply being exposed to admirable medical professionals appears to increase medical students’ empathy, and they actively seek out character-building relationships during their training. Future work will focus on whether the effect is stronger among individuals who enter med school with a higher level of sensitivity and moral development.
In earlier studies, Franzen spent three years looking at physicians’ moral disposition, role perceptions and patient interactions to determine their beliefs about “good doctoring.” In this recent research extending that line of inquiry to soon-to-be medical professionals, he used national data that followed the same students over about a year to evaluate how contact with professionals during their medical training influences and affects students’ moral elevation and, ultimately, the degree of empathy they bring to their professional lives.
His is the first study — “Beneficial Hidden Curriculum? The Role of Moral Elevation in Medical Socialization,” an article completed in 2020 that is currently under review by an academic journal — that applies the concept of moral elevation to med students. Sociologists use the term to describe the internal emotional response that one experiences when working with a supervisor, mentor or other role model who arrives at morally admirable decisions, especially when those decisions are difficult to make.
“Organizational role models hold an important place in the socialization process of individuals within organizations,” says Franzen. “Having a role model who displays interpersonal fairness and self-sacrificial leadership is related to increased attachment to and identification with the organization, as well as increased altruism. And those outcomes are mediated by moral elevation, which is, of course, desirable in the medical profession.”
Franzen, a quantitative sociologist, worked with a pre-existing dataset that he requested from colleagues at the Program on Medicine and Religion at the University of Chicago. The survey, titled Project on the Good Physician, asked questions focused on morality and compassionate care.
It used a multiple-choice format to ask respondents about, for example, how often they feel admiration for a physician, feel generous, feel open to others, or want to be like the physician they admire. It asked about the extent and nature of their sense of calling to the field, and their attitudes about medical educators’ possible roles beyond teaching the science of medicine.
The Project on the Good Physician includes 480 randomly selected medical students from two dozen schools nationwide. Franzen used the statistical analysis tool SAS to run two kinds of regression analysis coding dependent and independent variables to try to explain variance in how much people differed in their answers: logistic regressions to predict the odds of a respondent choosing one outcome or another, and linear regression to predict how much empathy increases, for example, for each increase in moral elevation.
The “hidden curriculum” of medical school is often tacitly taught via interactions with medical professionals who model how to be simultaneously empathetic and hardworking, Franzen says. Sometimes, it is a mentor in a structured relationship. But simply being around a person who displays admirable qualities has an impact. “The magnitude of the effect of moral elevation probably increases when it’s someone you have a direct relationship with, but in medical school it seems like it matters even in the absence of an actual relationship.”
And since med students often claim an increased sense of calling to be a physician, it’s no wonder that many of them desire teachers, supervisors and mentors who influence and solidify that calling with like-minded displays of meaning and purpose. In this they verify St. Augustine’s ancient tenet that “we imitate those whom we admire.”
“I found that the students who have higher levels of moral elevation are more likely to look for character shaping in medical school,” Franzen says, “and, in fact, they are more likely to say that they want their professors to train their character in a certain way.”
“Additionally, they’re more likely to judge the character of their fellow students because they’re more likely to be interested in good doctors as it relates to being a good person,” he continues. “So, if you’re a good person, then maybe you will also be a good doctor. But if you’re judged to not be a good person, these students have some concerns about how well you will do as a doctor.”
Franzen’s interest in this research has much to do with his many relationships with medical professionals (including his wife, who’s a pediatrician). He says roughly half of all medical students experience burnout at some point in their education, which can lead to depression. Other researchers have established that med students’ empathy levels can drop, too, especially during a student’s third year when clinical rotations and the official curriculum are life-consuming. If he can help shed light on how moral elevation can influence med students’ learning and life satisfaction during their stressful training, perhaps some of the negative circumstances of medical school could be staved off.
“Burnout is almost always the exact opposite of empathy,” Franzen explains. “It is the experience of depersonalization, whereas empathy is the ability to connect with other people effectively. So, I’m interested in some of those desirable outcomes for medical education and how it translates into patient care and patient interactions, but also in self-care. Because no one is healthy if we remove personhood from anyone: not the patient, of course, but also not the doctor.”
When it comes to empathy and morality in medical professionals, Franzen recognizes that “earlier character development matters quite a bit, too,” he says. That’s why he also started a study more than two years ago with Hope College students on the pre-health track who are preparing for advanced training and careers as nurses, doctors, physical therapists, dentists, veterinarians, and in other healthcare roles. A sizeable portion of each freshman class — this year, about a fifth — enter Hope planning to study for a healthcare profession. (And they do quite well! On average, for example, Hope’s medical school acceptance rate is more than 30% higher than the national average.)
Each spring since 2019, Franzen has sent a survey to those freshmen, asking them questions that measure moral foundations in humility, empathy, honesty and so on. With a 70% response rate so far, he is especially hopeful that this research will reveal even more about the change of virtues and character as one pursues a profession in the medical field, and provide him with baseline data to inform his ongoing work on medical socialization.
“Moral development and moral sensitivity are both usually required for good, empathetic connections,” Franzen says. “It seems so far as though those students who are more developed prior to med school tend to be most insulated from the loss of empathy, but also have the best rebound.”